In 2015, media reports alerted the U.S. Department of Health and Human Services Office for Civil Rights that a medical center in Florida had mishandled protected health information (PHI), exposing detailed personal and medical information about patients.
The OCR investigation uncovered some unsettling facts. The center waited four years to report that it had lost three boxes containing patient medical files. Its security was so lax that an employee sold patient information for five years before being detected.
The medical center paid $2.15 million to settle HIPAA violations, but atoning for the violation of medical ethics is harder. HIPAA is a set of rules governing healthcare that are based on long-established medical ethics. Responsible healthcare companies view compliance with HIPAA as an ethical requirement.
But what exactly are medical ethics? How does HIPAA fit into them? Let’s find out how you can enable compliance with both HIPAA and ethical standards.
What are medical ethics?
Medical ethics are the basic principles that guide every healthcare decision. The Hippocratic Oath is simple: First, do no harm. Avoiding harm is the first priority for every healthcare provider.
Medical ethics consists of four main principles, each of which affects HIPAA:
- Autonomy. Patients have the right to make their own decisions regarding their healthcare.
- Non-maleficence. Non-maleficence is the duty of medical practitioners to make certain their patients are never without care because of neglect.
- Beneficence. Beneficence is the obligation of healthcare providers and other professions to always make their patients’ well-being their highest concern.
- Justice. Justice requires giving all patients access to the treatments they need to heal.
Medical ethics are the core of HIPAA. Let’s work down that same list of medical ethical essentials to see how they apply to HIPAA:
- Autonomy. Under HIPAA, individuals control access to their information and how it’s used. Patients have the right, upon request, to their PHI.
- Non-maleficence. Identity theft causes serious harm. To protect patients from this harm, healthcare professionals must always handle PHI in accordance with HIPAA regulations. Establish procedures designed for HIPAA compliance and train your team to recognize the importance of following those procedures.
- Beneficence. A professionally operated healthcare business has an obligation to help patients get the most benefit from their PHI. Encourage your team to think about how to use the PHI you control to help patients. Could you make it easier for them to file insurance claims or coordinate medical appointments? Approaching business from that perspective will keep team morale high.
- Justice. HIPAA applies the same standards of privacy and security to each patient’s PHI and requires that covered entities do the same.
Breaching HIPAA regulations can land your business in serious financial trouble. A hospital was fined $85,000 for taking too long to send patients their medical information upon request. Failing to take seriously a patient’s legal rights under HIPAA is a violation of medical ethics that will damage your checkbook and your reputation.
Thankfully, you can be both legally and ethically compliant. Let’s discover how you can follow HIPAA regulations and medical ethics.
How embracing medical ethics aids in HIPAA compliance
While medical ethics are the heart of HIPAA, complying with HIPAA’s legal requirements requires procedures and training. Here are some basic guidelines for dealing with HIPAA in a way that embraces medical ethics:
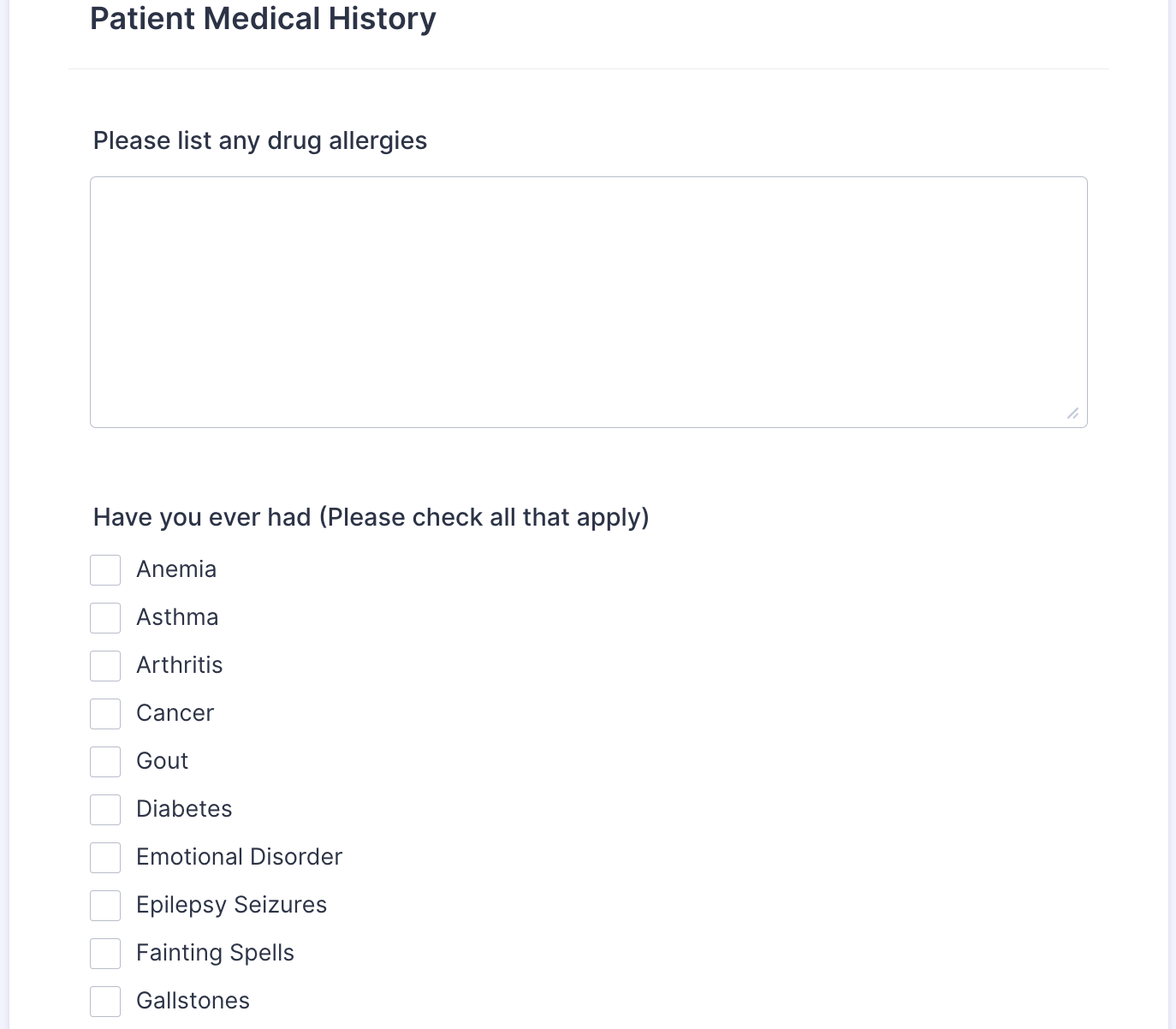
- Establish policies to protect PHI. Limit PHI access to staff with a direct need and the proper training in HIPAA and medical ethics. Jotform’s HIPAA-friendly online forms make it safe and easy for patients to input their PHI, and ensure that their information is secure.
- Understand PHI exceptions as required by law. Government agencies can legally demand access to PHI, without patient consent, such as with a warrant or court order. In certain circumstances you may be required to report information, such as a gunshot wound or signs of child abuse, regardless of patient consent.
- Recognize that patients have autonomy over their PHI. Patients are entitled to a paper copy of their medical information within 30 days of their initial request. Both HIPAA and medical ethics require you to promptly provide PHI to patients.
- Encrypt PHI when you send it electronically. End-to-end encryption keeps PHI secure until it gets to the right person.
- Appoint a HIPAA-friendly officer. Assign your compliance officer to monitor PHI procedures for HIPAA compliance. Make the compliance officer responsible for regularly updating data security software.
- Train your workers on HIPAA compliance. Employees must understand how HIPAA and medical ethics work together.
Health decisions made in compliance with HIPAA and medical ethics result in best healthcare possible. Combining HIPAA compliance with medical ethics protects individuals from identity theft and your business from lawsuits and fines. HIPAA compliance, at its root, is all about protecting a patient’s digital information and safety.









































































































Send Comment:
1 Comments:
More than a year ago
Grateful and thankful for a very informative and very clear presentation.