There are nearly 1,000 manufacturers of medical devices in the United States today. These companies make money by bringing new products to market. But before they can sell a new type of insulin pump or popularize the next generation of cochlear implants, they need to prove that their latest invention is safe and effective.
Proof comes from scientific studies — from research — and medical research requires human subjects. Studying people without their full agreement is illegal and unethical, so medical gatekeepers require researchers to obtain consent from their subjects before running a single experiment. That consent includes education — explaining everything the subject might need to know about their participation in the study. This combination of education and permission is called informed consent.
Informed consent is a mainstay of research within and beyond medicine. While all types of research projects involve human subjects and thereby require informed consent — a galaxy of social sciences, for instance — the medical product pipeline in the United States lets us observe informed consent within a broader commercial ecosystem. Let’s put it under the microscope and see what we can learn about informed consent in research.
Key participants in the informed consent process for research on medical devices
Informed consent is required for any medical research study. But who determines the requirements? And among the manufacturer’s staff, who’s in charge of it? Here are the major players involved in informed consent for commercial medical research.
1. The Food and Drug Administration (FDA)
The FDA regulates medical devices and — as the name implies — pharmaceutical companies in the United States. It requires informed consent for all the subjects of all the studies leading up to a product’s approval.
Since a federal regulatory agency enforces it, the FDA’s requirement for informed consent is written into law — the Code of Federal Regulations, Title 21, Volume 1, part 50, Subpart B, Section 50.20, to be exact.
2. Institutional Review Board (IRB)
The FDA requires researchers to work with a group that reviews research protocols — and informed consent documents — to make sure researchers are treating subjects properly. This organization is called an IRB.
Some institutions, like universities, operate their own IRBs. However, many medical device manufacturers contract with a local or regional IRB to fulfill the FDA’s regulatory requirements. Either way, the Office for Human Research Protections (OHRP) within the U.S. Department of Health and Human Services (HHS) must authorize the IRB.
That means the ultimate authority controlling informed consent requirements in medical research is the HHS, at least in the United States. The FDA is an agency within HHS, and HHS authorizes IRBs at every level. They all fit into each other like the pieces of a Russian doll, and researchers must pass their informed consent documentation through at least the inner two layers of the shell — their IRB and the FDA.
3. Regulatory affairs staff
The FDA and the IRB check to make sure researchers are following the rules. Regulatory affairs specialists are on the other side of the transaction, employed by the manufacturer that wants to bring a new medical product to market. It’s the job of regulatory affairs to work with the IRB to fulfill the FDA’s requirements — including those surrounding informed consent.
Marie Buharin is a regulatory affairs expert in medical devices and founder of the website Modernesse. She has worked in regulatory affairs departments for a decade. “Regulatory affairs is a specific position or a specific function in medical devices, pharmaceuticals, and biologics,” Buharin says. “We obtain FDA approval for these therapies.”
4. Clinical research organizations (CRO)
The “C” in “CRO” doesn’t just stand for “clinical,” as in “involving direct observation of the patient.” It also stands for “contract,” as in a business agreement. (The medical device industry accepts both terms.) CROs are companies that design and run medical studies for manufacturers.
A device manufacturer or a pharmaceutical company will hire a CRO to run the studies they need to get FDA approval for a product. Meanwhile, the regulatory affairs staff makes sure everyone complies with FDA regulations while working directly with the FDA and IRBs to keep the legal documentation clean. Keeping informed consent forms up to date is a big part of the job throughout the entire research process.
5. The principal investigator
Every clinical investigation needs a leader, someone who interacts directly with the subjects. That’s the principal investigator — “usually a physician who specializes in the research topic, depending on what the therapy is,” Buharin says. These doctors bring the CRO’s research protocols into the clinical setting, and they’re the patient’s main point of contact for informed consent discussions.
“The principal investigator’s office is responsible for physically obtaining a signature on the informed consent form as well as verbally explaining information to make sure the subjects understand what they’re signing,” Buharin says.
6. The subjects
The purpose of informed consent is to preserve the subject’s right to self-determination. The human subject of a medical study is the most important person in the informed consent process. In fact, study sponsors have a deep, vested interest in making sure that they inform the subject’s consent as much as possible.
“Manufacturers care about patient safety, and they want to ensure patients understand the risks and potential benefits of the clinical trial,” Buharin says. “And from a regulatory perspective, if you don’t obtain informed consent from the subject, you cannot use that subject’s information for your clinical investigation.”
This loss of data can sink a patent. “In medical devices, the studies are smaller than in pharmaceuticals,” Buharin says. You’re running 200-, 300-, 400-patient studies. If you fail to obtain informed consent from 20 of them, all of a sudden you only have 380 subjects to show the FDA that this is a safe and effective therapy, and they’re going to say, ‘What happened to the other 20?’ ”
So, if you don’t have informed consent, you don’t have data.
Elements of an informed consent form for medical device research
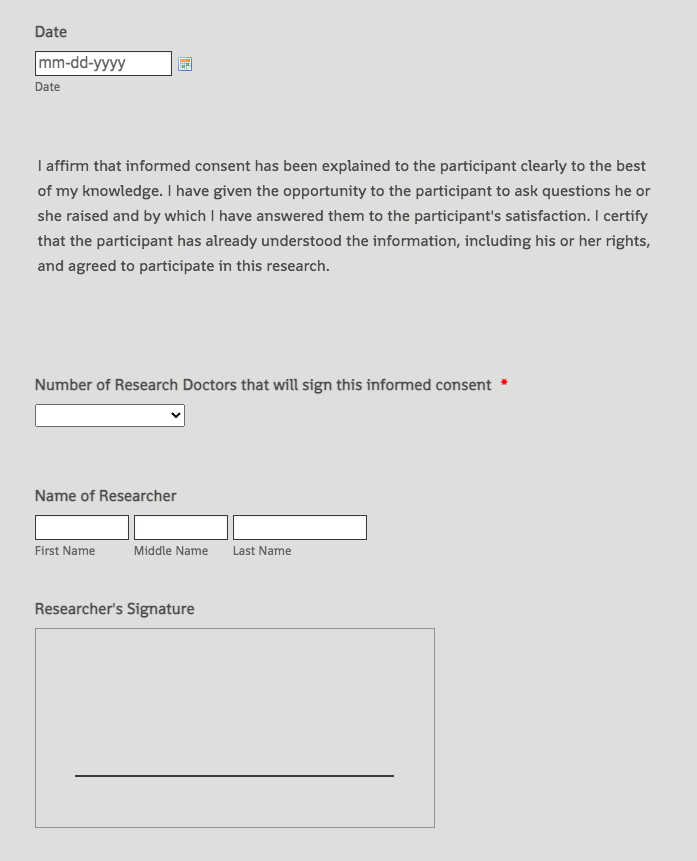
While informed consent is as much a conversation as a document, researchers do have to provide written proof of the patient’s knowledge and agreement. Those documents are the only way to prove that a subject is willingly participating in the study, and regulatory affairs teams spend a lot of time getting the forms right.
An informed consent document for a research study isn’t just a questionnaire. It’s a legal form — and not a simple one. “It’s quite a long document, which is why the verbal part of informed consent is also important, because people don’t sit around reading long legal documents,” Buharin says. “We’re talking about people’s health, so you really want to make sure they’re understanding what you’re communicating to them.”
Here are some of the major elements of a proper informed consent form for research on medical devices:
- An explanation of the research’s purpose, goal, and method.
- A list of risks. “You need to make it very clear that the medical treatment they’re receiving is not standard care,” Buharin says. “It’s under investigation, and there are risks you know as well as potential, unknown risks.” Researchers must disclose those.
- A list of benefits. The medical product has only reached the trial stage because its manufacturers believe it can help people; they must make those potential benefits clear.
- Confidentiality rights and agreements.
- Information about compensation — how much compensation subjects will receive and when.
- A list of contacts who can answer questions about the study. “Subjects need a contact for their principal investigator, who is the physician,” Buharin says. “They’ll also need a contact at the manufacturer, who’s the sponsor of the clinical investigation as well as potentially in the CRO.”
- A notice that participation is voluntary and can end at any time.
This isn’t a comprehensive list. For more information about what to include on an informed consent form for a clinical study, see this FDA resource. For sample forms, see Jotform’s informed consent template for research.
What medical staff should know about informed consent for research on medical devices
Anyone in the principal investigator’s office may end up with the job of collecting informed consent forms for a medical research study — or at least ensuring their successful processing. Administrators, assistants, nurses, and other physicians may all participate in informed consent. This is a serious job, as Buharin stresses.
“These are regulated forms. It’s really important to take the time to understand the information within them,” she says. “Reach out and ask questions, and make sure you understand the information before you start talking to subjects about it.”
According to Buharin, “A lot of these informed consent forms are for therapies you’ve probably never heard of or seen. They’re completely new treatments. And sometimes you might not be able to get all that detail just from reading legal-type language, so just make sure you speak to someone.”
Documentation is vital, but informed consent in research is, at its heart, a conversation.












Send Comment: