In theory, healthcare organizations will provide clear and thorough informed consent documents for their patients to sign. But in practice, one study found that the average quality score of an informed consent document on a scale of 0–20 ranges from 0.6 to 10.8.
Clearly, there’s room for improvement. Part of that improvement may require a better understanding of implied consent vs informed consent and the elements of informed consent.
What distinguishes implied consent from informed consent
There’s a major difference between implied consent and informed consent. With implied consent, the way a patient behaves indicates whether or not they give you permission to do something. There is no formal agreement. For example, a patient who calls to make an appointment is giving implied consent to treatment.
While implied consent is informal, informed consent is a legal term that requires seven elements to be valid:
- The individual is competent and can understand what they’re consenting to. For example, a patient with dementia may not give informed consent.
- The individual is making the decision voluntarily — i.e., no one is forcing them to do so.
- The patient has received sufficient information to make a decision. For instance, a patient with psoriasis has been offered a topical cream that will have minimal side effects as well as an oral medication that may compromise their immune system, and their healthcare provider has given them an explanation and information that describes the risks and benefits of both treatments.
- A plan has been recommended to the individual — e.g., the dermatologist has recommended that the psoriasis patient try the topical cream for eight weeks.
- The individual understands the terms being used in elements three and four.
- The individual has decided on a treatment — e.g., the topical cream.
- The treatment plan has been authorized.
If any of these elements aren’t met, informed consent has not been given. Healthcare providers are required to obtain informed consent before many medical procedures in nonemergency situations. If the patient is a minor, then the parents or legal guardians need to give informed consent.
The importance of informed consent
Generally, healthcare providers are required by law to obtain informed consent from their patients before beginning a course of treatment. There are a lot of procedures that don’t require a signed informed consent form from a patient, like prescribing a simple course of antibiotics.
If delaying treatment would result in irreparable harm or the patient’s death, you don’t need to obtain informed consent. For example, if a patient was brought into the emergency room unconscious with a severely ruptured spleen, a physician could operate on the patient without getting consent.
However, most surgeries, advanced medical tests — like endoscopies — chemotherapy, most vaccines, and high-risk treatments all require the patient to sign a form before treatment can begin. In many cases, you’ll also need written informed consent for telemedicine visits so that patients know about their privacy rights.
How to obtain written informed consent
When you get written informed consent from a patient, you have a documented record that the patient agreed to the treatment, even if they change their mind later. To do this, not only will you need to explain to the patient what they’re agreeing to and make sure they understand it, but you’ll also need to get a signed form to this effect.
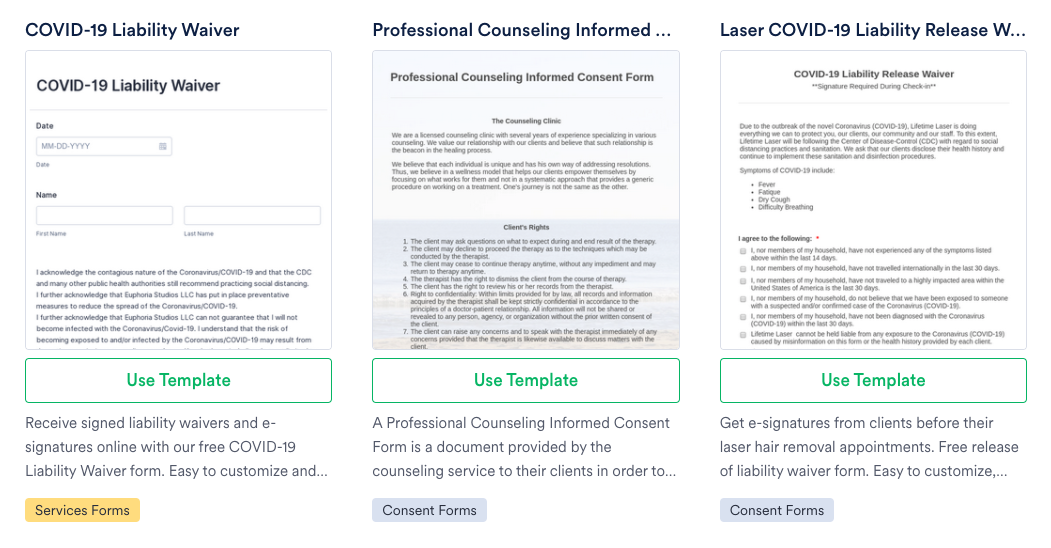
One of the easiest ways to do this is to use a Jotform informed consent form template. These prebuilt templates can be customized to your practice and signed electronically by the patient. You can create different forms for different procedures and include the risks of treatment for each.
When you customize your informed consent forms, make sure that you’re collecting basic information — like the patient’s name, address, date of birth, and medical history. In addition, include a section about the procedure that they’re having as well as a clause stating that the patient knows what they’re agreeing to.
One of the features that makes Jotform an easy way to collect informed consent is the electronic signature widget. This means you can send the informed consent form to the patient along with further information for them to review. Then when they’re in your office, they can ask questions and easily sign the form on a tablet or another device.
While getting implied consent is good enough for uncomplicated treatments and simple blood tests — like for cholesterol levels — when patients need more aggressive treatment or high-risk procedures, informed consent is necessary. Make sure it’s easy for both of you with a customized online form.













Send Comment: